A local research team has developed a ceramic-based ink that could allow surgeons to 3D-print bone-like structures containing living cells.
3D printers may one day become a permanent fixture in operating theatres after engineers and scientists from the University of New South Wales (UNSW) Sydney showed that the technology could be used to repair damaged bone tissue.
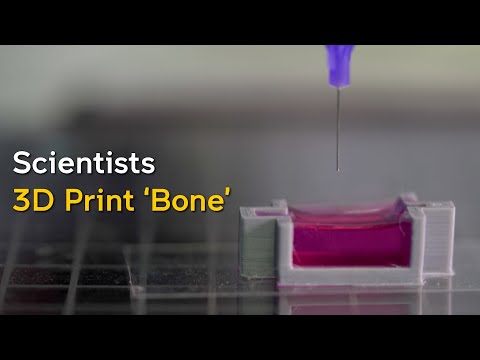
Using a 3D-printer that deploys a special ink made up of calcium phosphate, the team developed a new technique, known as ceramic omnidirectional bioprinting in cell-suspensions (COBICS), enabling them to print bone-like structures that harden in a matter of minutes when placed in water.
Postdoctoral research associate Sara Romanazzo told create that the team, led by biomedical engineer Dr Iman Roohani from UNSW’s School of Chemistry and Associate Professor Kristopher Kilian, came together to make a world-first breakthrough.
“Dr Roohani was working on developing a new biocompatible ceramic ink that sets within minutes. At the same time, Professor Kilian’s lab was working on a viscous bath to 3D print complex structures,” she said.
“I took on the task of combining the ink with the 3D printing technique, and explored the addition of living cells.”
Their discovery allowed the material to be created at room temperature — complete with living cells — and without harsh chemicals or radiation.
Eventually, it could have applications such as using the ink to create bone in the lab for disease modelling, as a bioactive material for dental restoration, or to direct bone reconstruction in a patient.
“The ink is a calcium phosphate paste with a specific formulation that allows the material to be used directly in an aqueous environment without the need for any post-processing steps, such as high temperature treatments, that are required for other types of existing ceramic materials,” Romanazzo said.
“Thanks to this property, the ink can be printed in direct contact with living cells, and this is the first time such a thing can be done.”
Serve at room temperature
The traditional technique for manufacturing such a substance in a laboratory, Killan said, is to produce a dry material that is washed profusely before adding living cells to it.
“The cool thing about our technique is you can just extrude it directly into a place where there are cells, like a cavity in a patient’s bone,” he said.
“We can go directly into the bone where there are cells, blood vessels and fat, and print a bone-like structure that already contains living cells, right in that area.”
When the ink is combined with a collagenous substance containing living cells, it enables in-situ fabrication of bone-like tissues. These may be suitable for bone tissue engineering applications, disease modelling, drug screening, and in-situ reconstruction of bone and osteochondral defects.
“The ink takes advantage of a setting mechanism through the local nanocrystallisation of its components in aqueous environments, converting the inorganic ink to mechanically interlocked bone apatite nanocrystals,” Roohani said.
“In other words, it forms a structure that is chemically similar to bone-building blocks. The ink is formulated in such a way that the conversion is quick, non-toxic in a biological environment and it only initiates when ink is exposed to the body fluids, providing an ample working time for the end-user, for example, surgeons.”
Exciting possibilities
While it’s early days, the bone-printing process could open up a whole new way of treating and repairing bone tissue, and the research team said there had been keen interest from surgeons and medical technology manufacturers.
“We have an ongoing animal study at the moment that will hopefully confirm our hypothesis that there should be no harmful components in our material. Thus far all of our tests with human cells in the laboratory have confirmed high biocompatibility,” Romanazzo said.
“We are now looking at large animal models to implant our material in, which should take about a year, in which case we hope to proceed with human trials and regulatory approval.
“If everything goes well and we find external funding support, we are optimistic the technique may be ready for the clinic within five years.”